You hear it all the time in the mortgage debate when dealing with the foreclosure mess and the plague of bogus affidavits and other legal documents: “we should not give some deadbeat a free home because they signed the mortgage notes and received the funds to buy their homes, so they must owe the money. I mean after all, you should not have borrowed money that you cannot repay!” How can those losers deny that they owe the money? That money is owed to someone; the mortgage notes are somewhere; and someone, somewhere actually and lawfully owns the notes. The real question is: Who?
Many of the people advancing these “free home” arguments are the same people that didn’t scream or shout when Wall Street stopped making money and the American taxpayer came to rescue with hundreds of billions of dollars to save their collective asses. After all, it was all just a mistake by the smartest guys in the room. These were the guys who failed to take into account that a lot of these adjustable rate mortgages might not perform once they adjusted. These were also the same people who assumed that the value of residential real estate would continue to appreciate forever at an annual rate of at least 15% per year.
Who exactly suggested that Florida or any other state for that matter is a pro borrower jurisdiction? The facts are that about 95% of the Florida foreclosure cases are won and homes are lost without a fight. The foreclosure attorneys don’t even come into court to get their summary judgments in many cases, they just call them in to the judge. These lawyers are very busy and due process and proper evidence are just technicalities to be overcome.
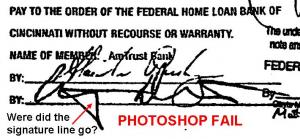
The banks in many cases cannot prove who owes money to whom, and so their law firms have been busy manufacturing the evidence needed.
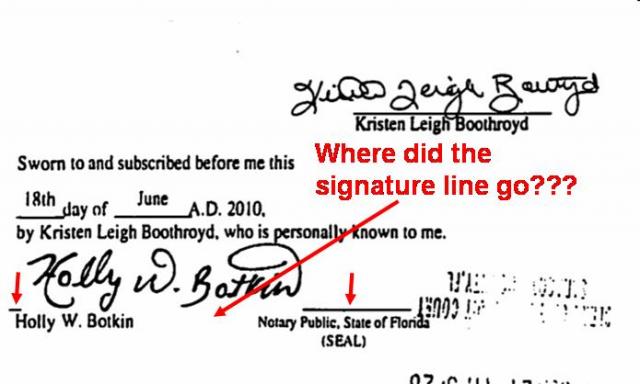
How about here, where the bank produced what was purported to be the same note twice, but with certain… irregularities:

If you can’t prove it, photoshop it:
Well, the Attorney General’s office of Florida has finally taken notice and is investigating the fraud that is occurring. It is about time. I wonder how many homes were illegally and fraudulently taken in the meantime?
A tip of the hat to 4closurefraud.org